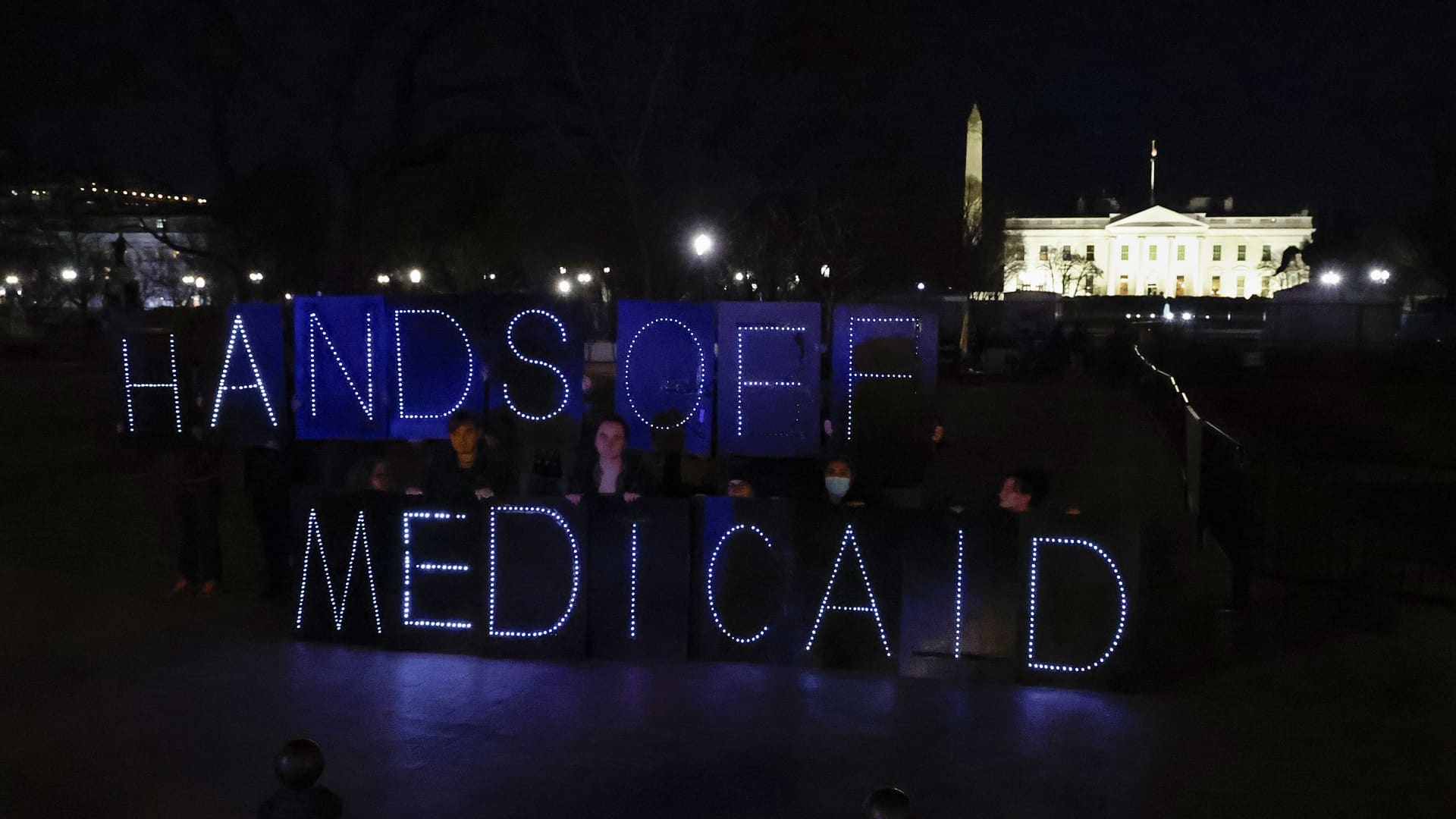
Protect Our Care supporters display “Hands Off Medicaid” message in front of the White House ahead of President Trump’s address to Congress on March 4 in Washington, D.C.
Paul Morigi | Getty Images Entertainment | Getty Images
Cuts to Medicaid will have to be on the menu if House Republicans want to meet their budget goals, the Congressional Budget Office said in a report this week.
The chamber’s budget blueprint includes $880 billion in spending cuts under the House Energy and Commerce Committee, which oversees the program.
Medicaid helps cover medical costs for people who have limited income and resources, as well as benefits not covered by Medicare such as nursing home care.
To curb Medicaid spending, experts say, lawmakers may choose to add work requirements. Doing so would make it so people have to meet certain thresholds, such as 80 hours of work per month, to qualify for Medicaid coverage.
Republicans have not yet suggested specific changes to Medicaid. However, a new KFF poll finds 6 in 10 Americans would support adding work requirements to the program.
More from Personal Finance:
DOGE layoffs may ‘overwhelm’ unemployment system
Education Department cuts leave student loan borrowers in the dark
Congress’ proposed Medicaid cuts may impact economy
Imposing work requirements may provide a portion of lawmakers’ targeted savings. In 2023, the Congressional Budget Office found implementing work requirements could save $109 billion over 10 years.
Yet that change could also put 36 million Medicaid enrollees at risk of losing their health-care coverage, estimates the Center on Budget and Policy Priorities. That represents about 44% of the approximately 80 million individuals who participate in the program. The estimates focus on adults ages 19 to 64, who would be most likely subject to a work requirement.
The idea of work requirements is not new. Lawmakers have proposed work hurdles to qualify for other safety net programs, including the Supplemental Nutrition Assistance Program, or SNAP.
The approach shows an ideological difference between the U.S. and European social democracies that accept a baseline responsibility to provide social safety nets, said Farah Khan, a fellow at Brookings Metro’s Center for Community Uplift.
“We view welfare as uniquely polarized based on which party comes into power,” Khan said.
When one party frames it as a moral failing to be poor because you haven’t worked hard enough, that ignores structural inequalities or systemic injustices that may have led individuals to those circumstances, she said.
Medicaid work requirements prompt coverage losses
Loss of coverage has been a common result in previous state attempts to add Medicare work requirements.
When Arkansas implemented a work requirement policy in 2018, around 1 in 4 people subject to the requirement, or around 18,000 people total, lost coverage in seven months before the program was stopped, according to the Center on Budget and Policy Priorities. When New Hampshire attempted to implement a work requirement policy with more flexible reporting requirements, 2 in 3 individuals were susceptible to being disenrolled after two months.
“Generally, Medicaid work requirements have resulted in coverage losses without incentivizing or increasing employment and are a policy that is really unnecessary and burdensome,” said Laura Harker, senior policy analyst at the Center on Budget and Policy Priorities.
The “administrative barriers and red tape” from work requirements broadly lead to coverage losses among both working individuals and those who are between jobs or exempt due to disabilities, illnesses or caretaking responsibilities, according to the Center on Budget and Policy Priorities.
Notably, around 9 in 10 Medicaid enrollees are already working or qualify for an exemption, Harker said.
Separate research from the American Enterprise Institute finds that in a given month, the majority of working-age people receiving Medicaid who do not have children do not work enough to meet an 80-hour-per-month requirement.
Consequently, if work requirements are imposed on nondisabled, working-age Medicaid recipients, that would affect a large number of people who are not currently in compliance, said Kevin Corinth, deputy director at the Center on Opportunity and Social Mobility at the American Enterprise Institute.
Either those individuals would increase their work to remain eligible or they wouldn’t, and they would be dropped off the program, Corinth said.
“If you put on work requirements, you’re going to affect a lot of people, which could be good or bad, depending on what your view of work requirements are,” Corinth said.
Lawmakers may also cut Medicaid in other ways: capping the amount of federal funds provided to state Medicaid programs; limiting the amount of federal money per Medicaid recipient; reducing available health services or eliminating coverage for certain groups.

 Economics1 week ago
Economics1 week ago
 Accounting1 week ago
Accounting1 week ago
 Economics1 week ago
Economics1 week ago
 Economics1 week ago
Economics1 week ago
 Economics1 week ago
Economics1 week ago
 Economics1 week ago
Economics1 week ago
 Personal Finance7 days ago
Personal Finance7 days ago
 Economics1 week ago
Economics1 week ago













