Two decades ago, a group of senior-housing executives came up with a way to raise revenue and reduce costs at assisted-living homes. Using stopwatches, they timed caregivers performing various tasks, from making beds to changing soiled briefs, and fed the information into a program they began using to determine staffing.
Personal Finance
Algorithms guide senior home staffing. Managers say care suffers.
Published
1 year agoon
At a Brookdale facility in Chicago, tiny elevators prevented residents from being herded en masse to dinner, necessitating more trips and more time than Service Alignment allotted. At a facility in New Port Richey, Fla., the algorithm recommended fewer caregivers than buildings, making it impossible to monitor all residents at all times. And at a facility near Fort Worth, residents often could not undress, shower and get dressed again within the allotted 20 minutes — constantly putting caregivers behind in their tasks.
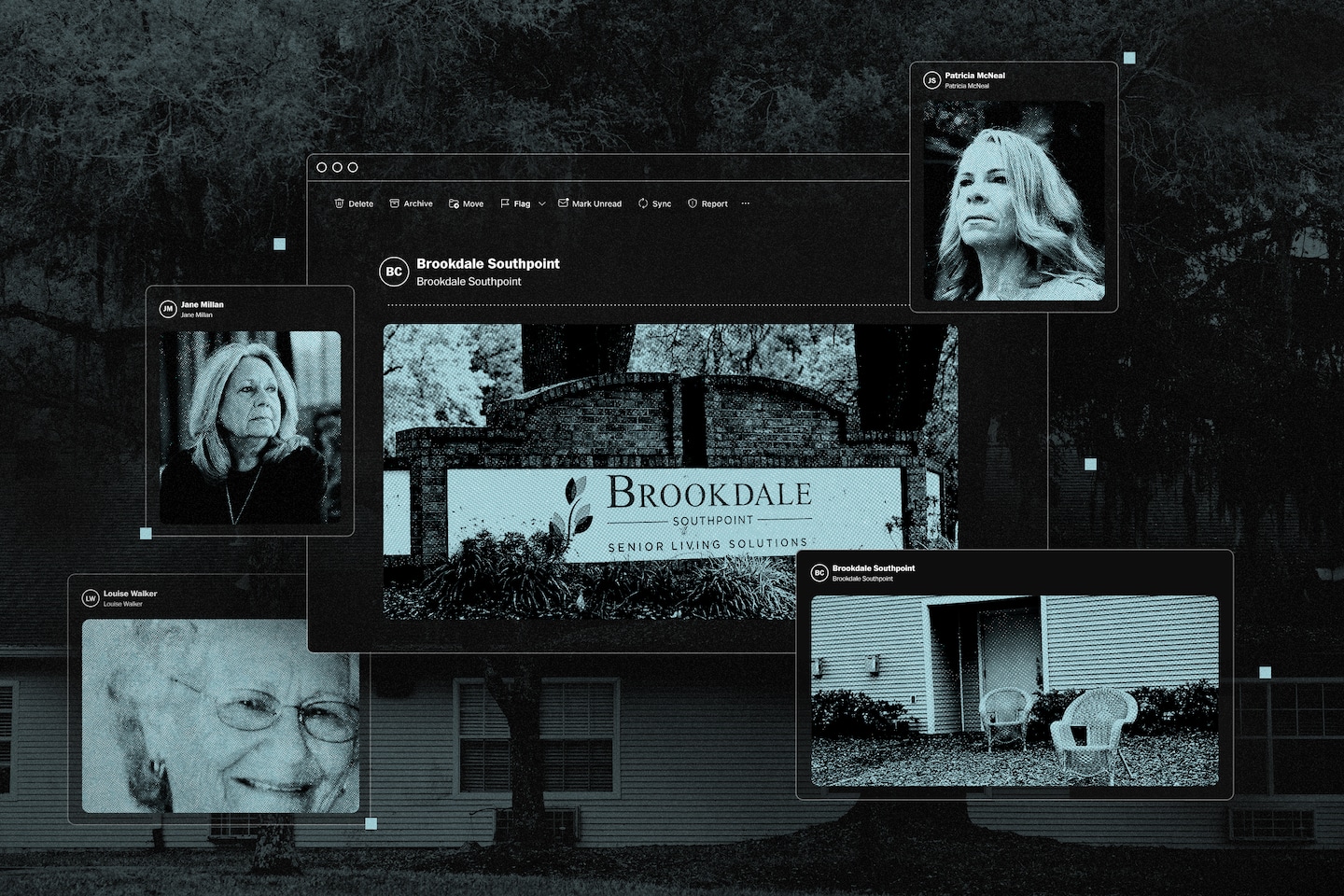
In emails and phone calls to Brookdale executives, building managers repeatedly complained that the company’s algorithm underestimated the amount of labor they needed to meet resident needs, according to court records, internal company documents reviewed by The Washington Post, and interviews with more than 35 current and former Brookdale employees. Several managers said they quit or were fired after objecting to the system, including Patricia McNeal, 53, who spent six years overseeing Brookdale facilities in Ohio and Florida.
“Brookdale is handing you this thing that says, ‘This is what it says you need, hire for that,’” McNeal said. “My eyes told me that we weren’t getting enough” staff to care for residents.
While assisted-living chains promote their properties like all-inclusive resorts with round-the-clock care, many operate more like assembly lines, where low-wage workers perform a series of discrete, predictable tasks, documents and interviews with industry veterans show. Brookdale, based in Brentwood, Tenn., pioneered staffing systems based on algorithmic formulas, an approach experts say is ill-suited to caring for the elderly, who are growing more frail and are more likely to suffer from chronic conditions than previous generations.
In two civil lawsuits against Brookdale — one in Tennessee, one in California — a dozen residents or relatives of residents claim they suffered due to short-staffing caused by an overreliance on algorithms. Sunrise Senior Living, a rival which in 2016 directed all of its facilities to follow its own staffing formula, is also defending a lawsuit by a group of customers who allege similar concerns. A spokeswoman for Sunrise declined to comment, citing pending litigation.
In a statement to The Post, Brookdale spokeswoman Jackie Dickson disputed the allegations in the lawsuits and said that Brookdale empowers local facility managers to set staffing levels as they see fit. Last year, a federal judge denied class-action certification for some of the claims in the California lawsuit, in part because plaintiffs failed to show that facilities are “similarly staffed.”
“Service Alignment is a resource offered to community leaders to assist them with appropriately staffing communities,” Dickson said. “This tool accounts for community-specific layouts and features, the ever-changing needs of residents, as well as applicable regulatory requirements, and is customized based on feedback from local community leaders.”
However, when the company began rolling the algorithm out to all its facilities, in 2013, then-CEO Andrew Smith told financial analysts one of the main goals was “to make sure that we don’t over-staff.”
In the fall of 2020, McNeal said she begged her superiors to send help as she scrambled to care for the rapidly declining health of residents in a Jacksonville facility she managed during the covid pandemic. When help didn’t arrive, McNeal scheduled additional workers as “training” staff without company approval — an action for which Brookdale fired her, documents show, saying she didn’t “demonstrate good stewardship to the company’s resources.”
A few weeks after her termination, Louise Walker, 89, died after falling in her room at the Jacksonville facility. State investigators cited Brookdale for medical neglect, saying workers failed to adequately supervise Walker, a high fall risk who was diagnosed with dementia. At the time, two employees were tending to more than a dozen residents in the dementia care unit, and neither had training on traumatic brain injuries, court records show.
“I don’t blame a lot of the people who work there,” said Jane Millan, 72, Walker’s daughter, whose wrongful-death lawsuit against Brookdale is set for trial in May. “They don’t have enough staff to do the duties they have to do, so something has got to slide.”
Dickson, the Brookdale spokesperson, said McNeal’s account is “inaccurate” but declined to comment on confidential employment matters. She said the company denies any wrongdoing in Walker’s death and declined further comment, citing the litigation.
There are no federal laws regulating assisted-living facilities, and only 13 states require staffing minimums. Brookdale says its algorithm sets staffing levels above statutory minimums in states that require them — a claim disputed by plaintiffs in the Tennessee lawsuit, which has requested class-action certification.
Using time sheet data provided by Brookdale covering seven facilities in North Carolina, an expert for the plaintiffs found that all failed to meet the state’s clinical care staffing minimums during at least 10 percent of shifts from 2016 to 2022. Four facilities fell short of state minimums during at least one out of every three shifts.
An expert hired by Brookdale said in a court filing that the North Carolina analysis failed to account for employees who clock in under one department, such as a cook, but then contributed to caregiving tasks when they had extra time.
In the California lawsuit, relatives of Brookdale residents claimed understaffing contributed to their loved ones being found covered in feces, breaking bones or wandering away unattended. One woman was hospitalized for extreme dehydration because staff had left food and water outside her door for three days straight without checking to see if she consumed any of it, according to her son, who provided a sworn statement in the lawsuit.
The case is scheduled for trial in October.
On Christmas Day 2020, a man was found lying facedown in the courtyard of a Brookdale facility in Destin, Fla. — frozen to death after being left unattended for more than 12 hours, a police investigation found. A caregiver working there that day told police the facility was unsafe because “the staff to resident ratio is horrible” and “they need to have more people working in the facility to keep up” with residents. She said she raised her concerns with Brookdale executives and “nothing was done,” according to the police report. It’s unclear whether this incident led to a lawsuit or whether the company’s algorithm played any role.
Dickson declined to comment on individual residents or facilities but said Brookdale is regularly cited by industry surveys as having high customer satisfaction.

“Brookdale needs to get
rid of Service Alignment
and get more staff in here
on each shift… It’s not
safe and it’s not right.
Something bad is going
to happen and I just
don’twant to be here
when that happens.”
June 2021 email from Virginia Steinman,
former health andwellness director at
Brookdale Morehead City, North Carolina


“Brookdale needs to get rid of Service
Alignment and get more staff in here on
each shift… It’s not safe and it’s not right.
Something bad is going to happen and I just don’t want to be here when that happens.”
June 2021 email from Virginia Steinman, former health and
wellness director at Brookdale Morehead City, North Carolina
The problems of understaffing and questionable levels of care pervade the assisted-living industry. Since 2018, more than 100 residents died after wandering away from such facilities or being left unattended outside, a Post investigation found.
Brookdale, Sunrise and Atria Senior Living, another top chain, were questioned as part of a congressional committee inquiry into concerns about the costs and quality of care at senior living facilities raised by The Post’s reporting. A spokesman for Sen. Bob Casey (D-Pa.), chairman of the Senate’s Special Committee on Aging, said the companies provided some responses to the lawmakers’ questions but the committee has declined to make them public. A spokesperson for Atria said the company prioritizes the safety and well-being of residents.
Brookdale became the industry giant through a wave of mergers between 2005 and 2014. Among them was Alterra Healthcare, which had invented the system for determining staff levels based on stopwatch studies. Brookdale believed the program could help it rein in ballooning expenses and manage its growing empire from afar, according to interviews with former executives and transcripts of the company’s quarterly earnings calls with analysts.
It began rolling out Service Alignment to all its properties between 2013 and 2016 — during which its portfolio ballooned to nearly 1,200 senior homes — executives said on earnings calls. Under the new system, Brookdale would assess the health of every resident and determine exactly which tasks were needed to meet their needs. Using these assessments and the stopwatch time studies, the algorithm promised to tell building managers exactly how many minutes were needed to care for all residents each shift — and, therefore, the number of employees they were permitted to schedule.
Businesses have been timing tasks to improve worker efficiency for over a century. Frederick Taylor, one of the fathers of management consulting, devised the first time study in the late 1800s, when he noticed workers at a steel mill were intentionally doing as little work as they could, said Naren Agrawal, a professor of supply chain management and analytics at Santa Clara University. By understanding the times it took to perform individual tasks, businesses could catch workers who were slacking off and get a clearer picture of the total labor needed to build a product or perform a service, Agrawal said.
Such rigid systems can fail for tasks with wide variability, said Carri Chan, a Columbia Business School professor who researches health-care management and operations. “When you are taking care of patients, all of whom have unique needs, there is going to be a lot of variation,” she said.
In interviews, McNeal and nine other former executive directors of Brookdale facilities said Service Alignment failed to capture the complexities of working with seniors with cognitive decline. For instance, helping dementia patients take showers may take two or three times as long as other residents, because they often refuse to get undressed in front of caregivers they may not remember and need to be patiently guided through the process.
Each time a caregiver runs over time in one task, it takes away from the total caregiving hours for the entire building. As a result, some residents go without showers, rooms are left uncleaned and people needing close supervision are ignored, some of the former managers said.
When Service Alignment was rolled out, the algorithm forced many Brookdale facilities to reduce their staff, documents and interviews show. At other facilities, where the algorithm suggested more staff was needed, Brookdale intervened.

“We are talking about
missing showers and
time gaps on putting
residents in their beds
… I am wide awake at
night thinking about
anything else that may
get overlooked…
I cannot stress to
you how bad it is…
I am asking for help?
August 2021 email from Brenda Jarmer,
district director of operations in Florida.
In a message to The Post, Jarmer said
she wrote that email amid staffing
challenges brought on by the COVID
pandemic and that she believes Brookdale,
where she still works, is a “great company.”


“We are talking about missing showers
and time gaps on putting residents in
their beds… I am wide awake at night
thinking about anything else that may
get overlooked… I cannot stress to you
how bad it is… I am asking for help.”
August 2021 email from Brenda Jarmer, district director of operations in Florida.
In a message to The Post, Jarmer said she wrote that email amid staffing challenges
brought on by the COVID pandemic and that she believes Brookdale,
where she still works, is a “great company.”
Kelly Rubin, a senior director overseeing the staffing system, sent an email to regional managers warning of the likelihood the algorithm would show “favorable variances” in needed labor for some facilities — meaning, they needed more staff. Rubin said no facility would be granted more than two additional full-time employees, regardless of what the algorithm said.
“Just by virtue of flipping a switch from one platform to another does not justify additional labor because the platforms calculate differently,” Rubin wrote in the email, which, like other internal communications quoted in this story, was made public as part of a court record.
Rubin, who still works at Brookdale, said in a message to The Post that Brookdale tended to staff facilities at a “higher level” than the roughly 500 newly acquired properties that it was moving onto Service Alignment so she expected staff increases. Her message was intended to help local managers “evaluate the new platform’s guidance and make any adjustments they felt appropriate based on actual resident needs.”
Staff complaints started pouring in.
In 2016, Sarah Jenkins, a night-shift medication technician at a Brookdale in Jensen Beach, Fla., complained to the company’s internal tip line that short staffing was causing caregivers to cut corners, according to notes from the call included in a court record. Jenkins said her co-workers were applying wet-wipes to residents in lieu of giving them showers and set the thermostat to 64 degrees “because it keeps the residents in bed.” Jenkins, who no longer works for Brookdale, did not respond to a request for comment.
The following year, Jackie Smedley, a divisional director of sales and marketing, emailed a regional manager that “extreme action” was needed to improve resident safety at a facility in Clearwater, Fla., that was “very short on care staff” and had “no clinical oversight.” A resident had arrived at an emergency room with impacted fecal matter stuck to his skin. “The ER reported to Brookdale that this was the worst case of resident abuse they ever witnessed,” she wrote in an email that was included in court papers. Smedley, who no longer works for Brookdale, declined to comment.
Brookdale managers who scheduled more employees than the algorithm advised were required to propose a plan of correction, former employees said. Repeat offenders risked losing portions of their annual bonus. Brookdale’s Dickson called the employees’ description of these practices “inaccurate” but declined to elaborate.
Some managers told their bosses that Service Alignment assumptions must be wrong and asked for exceptions — which they sometimes got.
One example was the facility in Chicago with the small elevators. After sending someone to the building to study transport times, Brookdale agreed to reinstate the staffing level before Service Alignment, according to one of the building’s former managers, who declined to be named because they still work in the industry.

“I am concerned about
the safety and welfare
of our current residents.
If we can’t meet the needs
of current residents,
how can we meet the
needs of new residents?”
July 2017 email from Jackie Smedley,
formersoutheast divisional director
of sales and marketing


“I am concerned about the safety and
welfare of our current residents. If we can’t
meet the needs of current residents, how can
we meet the needs of new residents?”
July 2017 email from Jackie Smedley, former
southeast divisional director of sales and marketing
Other managers said their warnings were not heeded. Greg Brown quit three months after taking a job heading a Brookdale facility in Denver in 2019 because, he said, the algorithm didn’t recognize there were four different buildings and that leaving some of the buildings unattended would be dangerous.
“I quickly realized and explained in my resignation that I didn’t feel they were staffing the community in a correct and safe manner and that I wouldn’t be able to continue,” Brown, who has worked at various senior living homes for over 15 years, said in a direct message on LinkedIn. Brookdale no longer owns the property.
Brookdale’s solution to the wide variation in resident conditions was to charge more when they needed more time for any task than Service Alignment allotted. For example, if a resident routinely took long showers, caregivers were supposed to report that to their managers, who would reassess the resident’s needs, potentially increasing fees.
However, many employees found it difficult to constantly raise prices on the residents with whom they worked every day and who already were paying steep fees, said Saralyn Kerrigan, who ran a Brookdale building in Connecticut from 2011 to 2014.
“Rather than it being like advocating for seniors, making sure they had what they need, it became, what more could we get out of them?” Kerrigan said. “We were really encouraged to be upselling.”
Brookdale charged an extra $156 a month for residents who needed help laying out their clothes and toiletries in the morning, and an extra $703 a month if a resident routinely wandered the hallways and required periodic redirection, according to a pricing sheet for one Texas facility the company provided in a court filing this year.
At one facility earlier this year, Brookdale charged each customer with special cognitive or psychological needs an extra $468 to $703 a month for what averaged to about 14 minutes of additional care per day, according to a daily Service Alignment plan reviewed by The Post. The Post analysis was based on the total number of minutes Brookdale’s algorithm allocated for dementia-related assistance, divided by the number of people in the facility billed for those services.
As managers struggled under the new staffing system, the company’s finances got worse. More than three-quarters of Americans 50 and older want to remain in their homes for the long term, according to a 2021 survey by AARP — a number that has remained constant for more than a decade despite the industry’s marketing efforts and the aging of the nation’s demographics. Until recently, that trend left Brookdale and other industry leaders with too many buildings and not enough residents.
Brookdale lost money in each of the past 19 years except 2020, and its stock price, which peaked at $53 a share in 2006, has petered to just $7.
When McNeal started at Brookdale Southpoint in January 2020, the Jacksonville facility already had difficulty caring for its residents.
The one-story building, sandwiched between a busy intersection and a small pond in a commercial neighborhood south of the city, had been cited by regulators in 2018 for failing to properly supervise a misbehaving male resident who forced his way into the beds of female residents, state documents show. An employee interviewed by state inspectors at the time said “she felt there is nothing they can do to stop him because he is ‘out of his mind’ and he does not understand,” the inspector wrote in the report.
Adding to McNeal’s challenges, covid lockdowns forced residents to spend most of their days alone in their rooms, causing some to rapidly decline. One man became so disoriented he was peeling linoleum off the floor of his room and eating it, McNeal said.
Brookdale Southpoint typically had two to three caregivers assisting more than a dozen residents of the locked memory care unit and another one to two serving more than a dozen additional assisted-living residents, according to former employees and facility records. Because the building had very few dedicated housekeepers and dining staff, caregivers also had to do laundry, clean rooms and help serve meals in between making their rounds delivering medicine and assisting residents with grooming, bathing and going to the bathroom.
Brookdale has defended its practice of “universal caregivers” combining these roles as innovative and efficient. “You’re trying to find useful things that the associates can do overnight, in addition to ensuring that the residents are safe and cared for,” Smith, the former Brookdale CEO, said on a call with financial analysts in 2013. But as residents and their families have discovered, the wide-ranging responsibilities of these workers can take away from their ability to complete their caregiving duties.
A few months after starting at Brookdale Southpoint, McNeal said she discovered that a memory care resident wandered outside at about 11:30 p.m. while her caregiver was doing laundry. The resident remained alone in a wooded area until she was found at close to 7 a.m. the next day.
McNeal said she repeatedly pushed for additional help in conversations with her managers. Several times, Brookdale sent people to help McNeal conduct new health assessments of her residents, but each time, she said, it did not result in her facility getting more hours for additional employees.
Walker, the resident who died at Brookdale Southpoint, moved into the facility in June 2020 and paid $4,650 per month. In April 2021, Walker’s great-granddaughter, Brandi Faison, came by to give her Nannie a pedicure and was startled by the sight of her feet — hardened, yellow and cracking, with thick, curling toenails three to four times their normal length. She was so horrified that she took a photo and shared it with her family, and later shared it with The Post.
Walker, embarrassed by her appearance, told her great-granddaughter that “nobody ever came” to do her nails, Faison recalled.
Shortly after McNeal was fired, a Brookdale caregiver discovered Walker bleeding on the floor of her room. A police investigation found she had been left alone for two hours and 40 minutes, despite a facility policy of checking residents at least every two hours. Walker required extra attention due to “difficulty standing, ambulating, and safely functioning” on her own, according to a nurse practitioner’s note.
Though the hospital was a two-minute drive across the street, Walker was not received by the emergency room until nearly two hours after she was discovered, documents show. She died of a brain hemorrhage four days later. In their report, state investigators cited Brookdale’s failure to properly supervise Walker and the facility’s slow response time as evidence of neglect.
The night of Walker’s fall, the medication technician on duty had been allowed to go home early, leaving Marie Berleus — a Haitian immigrant who spoke limited English working her fourth 12-hour graveyard shift of the week — to puzzle through the medical crisis. Berleus exchanged text messages with her boss and searched for paperwork before finally calling a non-emergency ambulance service, rather than 911, 40 minutes after finding Walker, according to court records from a lawsuit Walker’s family filed against Brookdale. Berleus did not respond to a request for comment.
In court records, Brookdale’s lawyers denied that any of the facility’s actions caused Walker’s death, pointing out that a medical expert hired by the family could not say that a quicker response would have necessarily saved her life.
“I’m so tired,” Berleus wrote in one of her text messages to her boss that night.
The Washington Post is continuing to report on the assisted-living industry, and we want to know your experiences with elder care, assisted living and dementia care. Tell us about your experience here.
You may like
Personal Finance
You have options if you can’t pay your taxes by April 15
Published
10 hours agoon
April 11, 2025
Fotostorm | E+ | Getty Images
The tax deadline is days away — and the IRS is urging taxpayers to file returns on time and “pay as much as they can.”
However, if you can’t cover your total tax balance, there are options for the remaining taxes owed, according to the agency.
For most tax filers, April 15 is the due date for federal returns and taxes. But your federal deadline could be later if your state or county was impacted by a natural disaster.
If you are in the military stationed abroad or are in a combat zone during the tax filing season, you may qualify for certain automatic extensions related to the filing and paying of your federal income taxes.
Additionally, those living and working abroad also have extra time to file.
More from Personal Finance:
See if you qualify for the $1,400 IRS stimulus check before the deadline
Majority of Americans are financially stressed from tariff turmoil: CNBC survey
3 likely student loan changes as Trump looks to overhaul $1.6 trillion system
If you’re missing tax forms or need more time, You can file a tax extension by April 15, which pushes the federal filing deadline to Oct. 15.
But “it’s an extension to file, not an extension to pay,” said Jo Anna Fellon, managing director at financial services firm CBIZ.
File by April 15 and ‘pay what you can’
If you can’t cover your balance by April 15, you should still file your return to avoid a higher IRS penalty, experts say.
The failure-to-file penalty is 5% of unpaid taxes per month or partial month, capped at 25%.
By comparison, the failure-to-pay penalty is 0.5% of taxes owed per month, limited to 25%. Both penalties incur interest, which is currently 7% for individuals.
File on time and pay what you can.
Misty Erickson
Tax content manager at the National Association of Tax Professionals
“File on time and pay what you can,” said Misty Erickson, tax content manager at the National Association of Tax Professionals. “You’re going to reduce penalties and interest.”
Don’t panic if you can’t cover the full balance by April 15 because you may have payment options, she said.
“The IRS wants to work with you,” Erickson added.
Options if you can’t pay your taxes
“Most individual taxpayers can qualify for a payment plan,” the IRS said in a recent news release.
The “quickest and easiest way” to sign up is by using the online payment agreement, which may include a setup fee, according to the agency.
These payment options include:
- Short-term payment plan: This may be available if you owe less than $100,000 including tax, penalties and interest. You have up to 180 days to pay in full.
- Long-term payment plan: You’ll have this option if your balance is less than $50,000 including tax, penalties and interest. The monthly payment timeline is up to the IRS “collection statute,” which is typically 10 years.
The agency has recently revamped payment plans, to make the program “easier and more accessible.”

Personal Finance
Regulated finance needs to build trust with Gen Z
Published
12 hours agoon
April 11, 2025

Misinformation and lack of trust in traditional institutions runs rampant in our society.
The regulated financial sector is no different, particularly among young people. Roughly 38% of Gen Zers get financial information from YouTube, and 33% from TikTok, according to a recent Schwab survey.
As a former regulator and author of kids’ books about money, I am truly horrified by the toxic advice they are getting from these unqualified “finfluencers” — advice which, if followed, could cause lasting damage to their financial futures.
Most troubling are finfluencers who encourage young people to borrow. A central theme is that “chumps” earn money by working hard and that rich people make money with debt. They supposedly get rich by borrowing large sums and investing the cash in assets they expect to increase in value or produce income which can cover their loans and also net a tidy profit.
Of course, the finfluencers can be a little vague about how the average person can find these wondrous investments that will pay off their debt for them. Volatile, risky investments — tech stocks, crypto, precious metals, commercial real estate — are commonly mentioned.
‘The road to quick ruin’ for inexperienced investors
Contrary to their assertions, these finfluencers are not peddling anything new or revelatory. It’s simply borrowing to speculate.
For centuries, that strategy has been pursued by inexperienced investors as the path to quick riches, when in reality, it’s the road to quick ruin. There is always “smart money” on the other side of their transactions, ready to take advantage of them. For young people just starting out, with limited incomes and tight budgets, it’s the last thing they should be doing with their precious cash.
More from Your Money:
Here’s a look at more stories on how to manage, grow and protect your money for the years ahead.
Debt glorification is not the only bad advice being peddled on the internet.
You can find finfluencers advising against diversified, low fee stock funds in favor of active trading (without disclosing research consistently showing active trading’s inferior returns). Or ones that discourage individual retirement accounts and 401(k) plans as savings vehicles in favor of real estate or business startups (without mentioning lost tax benefits as well as the heavy costs and expertise needed to manage real estate or high failure rates among young companies).
Some encourage making minimum payments on credit cards to free up money for speculative investments (without mentioning the hefty interest costs of carrying credit card balances which compound daily).
Why are so many young people turning to these unqualified social media personalities for help in managing their money instead of regulated and trained finance professionals?
One reason: the finfluencers make their advice entertaining. It may be wrong, but it’s short and punchy. Materials provided by regulated financial service providers can sometimes be dry and technical.
Where to get trustworthy money advice
Xavier Lorenzo | Moment | Getty Images
They may be boring, but regulated institutions are still the best resource for young people to get basic, free information.
FDIC-insured banks can explain to them how to open checking and savings accounts and avoid unnecessary fees. Any major brokerage firm can walk through how to set up a retirement saving account. It’s part of their function to explain their products and services, and they have regulators overseeing how they do it.
In addition, regulators themselves offer educational resources directly to the public. For young adults, one of the most widely used is Money Smart, offered by the Federal Deposit Insurance Corporation — an agency I once proudly chaired.
There are also many excellent regulated and certified financial planners. However, most young people will not have the budget to pay for financial advice.
They don’t have to if they just keep it simple: set a budget, stick to it, save regularly, and start investing for retirement early in a low-fee, well-diversified stock index fund. They should minimize their use of financial products and services. The more accounts and credit cards they use, the harder it will be to keep track of their money.
Above all, they should ignore unqualified “finfluencers.”
Check their credentials. Question their motives. Most are probably trying to build ad revenue or sell financial products. In the case of celebrities, find out who’s paying them (because most likely, someone is).
Regulated finance needs to reclaim its status as a more trustworthy source for advice. The best way to do that is, well, provide good advice. Every time a young adult is burnt by surprise bank fees, seduced into over borrowing by a misleading credit card offer, or told to put their retirement savings into a high fee, underperforming fund, they lose trust.
I know regulation and oversight are out of favor these days. But we need a way to keep out the bad actors, and practices to protect young people new to the financial world. It’s important to their financial futures and the future of the industry as well.
Sheila Bair is former Chair of the FDIC, author of the Money Tales book series, and the upcoming “How Not to Lose $1 Million” for teens. She is a member of CNBC’s Global Financial Wellness Advisory Board.
Personal Finance
Is this a good time to buy gold? Experts weigh in
Published
13 hours agoon
April 11, 2025

Gold is often considered a safe-haven investment because it typically acts as a hedge in times of political and financial uncertainty. Prices are currently soaring amid fears of a global trade war and its potential to push the U.S. economy into recession.
However, some analysts think gold prices may have peaked.
“We’re probably close to maximum optimism on gold at this point,” said Sameer Samana, head of global equities and real assets at the Wells Fargo Investment Institute. Investors who chase returns may find themselves regretting it later.
“It’s so overbought,” Samana said. “Buying gold right now, you’re coming a little late to the party. It doesn’t mean it’s over, but you’re not early.”
So far this year, gold prices have notched more than a dozen record highs and are currently trading above $3,000.
Gold prices pop on tariff escalation
Gold futures prices were up about 21% year-to-date as of noon ET on Friday and 30% higher compared to the price a year ago. Prices have popped about 7% this week alone, on pace for the best week since March 2020.
By comparison, the S&P 500 is down about 11% in 2025 and up about 1% in the past year.
President Donald Trump imposed steep country-specific tariffs on Wednesday, but ultimately delayed them for 90 days. However, a trade war between the U.S. and China — our third-largest trade partner — escalated as each nation engaged in a tit-for-tat tariff increase.
As of Friday morning, the U.S. had put a 145% tariff on imports from China, which hit back with a 125% levy on U.S. goods.
While some analysts think gold prices are close to topping out, others think there’s room to run.
“Even though gold prices are at an all-time high, the reality is that in the next couple of years it could accelerate,” said Jordan Roy-Byrne, founder of The Daily Gold, an online resource for gold, silver and mining stocks.
How to invest in gold
Akos Stiller/Bloomberg via Getty Images
Experts often recommend getting investment exposure to gold through an exchange-traded fund that tracks the price of physical gold, as part of a well-diversified portfolio, rather than buying actual gold coins or bars.
“For most [investors], I would say a gold bullion-backed ETF makes the most sense,” Samana said. SPDR Gold Shares (GLD) and iShares Gold Trust (IAU) are the two largest gold ETFs, according to ETF.com.
Financial advisors generally recommend limiting gold exposure to the low-single-digit percentage, perhaps up to 3% or so, of one’s overall portfolio.
Gold tends to perform “okay” when investors are worried about inflation or stagflation, Samana said — fears sparked by the Trump administration’s recent tariff policies. However, it “rarely does well” during recessions, which is when bonds “really show their value,” he said.
Buying physical gold
Alternatively, buying physical gold, or bullion, including bars and coins, “is a financial insurance position, as opposed to part of your portfolio,” explained Roy-Byrne.
Consumers, especially, seem to like that idea. When Costco started selling 1-ounce bars last year, revenue soared, with Wells Fargo analysts estimating that the wholesaler generated up to $200 million a month from gold sales alone.

“Amidst the recent stock market turbulence, we’re seeing renewed interest in tangible, physical assets that exist outside traditional financial structures,” according to Tim Schmidt, the founder of Gold IRA Custodians, an online resource for buying gold.
But buying physical gold during uncertain times may not make much sense for investors unless they are extremely anxious the financial system might implode — at which point physical gold can theoretically help people barter for goods and services, Samana said.
Buying gold jewelry
Fine jewelry is a different story. The baseline value of gold jewelry is tied to its precious metal content, according to Schmidt. Higher-karat pieces, or 18K and up, contain more precious metal and typically retain value better, though they may be less durable for everyday wear.
“High-quality jewelry … can offer both personal enjoyment and potential financial benefits when selected carefully,” he said.
Craftsmanship and artistry also play a key role in pieces that could appreciate over time, particularly with hallmarks from top brands, such as Cartier, Van Cleef & Arpels and Tiffany & Co.
Buying gold right now, you’re coming a little late to the party. It doesn’t mean it’s over, but you’re not early.
Sameer Samana
head of global equities and real assets at the Wells Fargo Investment Institute
One year ago, Tiffany’s chief executive officer Anthony Ledru said high-quality jewelry may even be considered “recession proof.”
“People have been investing in jewelry since ancient times,” Schmidt said. “There’s something psychologically reassuring about holding an investment in your hand, especially during periods when markets seem disconnected from economic realities.”
What financial advisors say about gold
Gold prices extended their gains on Wednesday, following a record high in the previous session, as investors sought the comfort of the safe-haven metal in anticipation of the potential impact of U.S. reciprocal tariffs.
Akos Stiller | Bloomberg | Getty Images
“We have clients who currently hold positions in gold. These are typically individuals with substantial assets across various industries and sectors, using gold as a means of portfolio diversification and balance,” said Winnie Sun, co-founder and managing director of Sun Group Wealth Partners, based in Irvine, California.
Even in the face of heightened uncertainty largely due to tariff-induced market swings, “we are not proactively recommending that clients add to their gold positions at this time,” said Sun, a member of CNBC’s Financial Advisor Council. “Instead, we suggest maintaining higher cash reserves, fully funding emergency savings, and reallocating as needed based on evolving financial goals.”
Lee Baker, a CFP based in Atlanta, says more clients are worried that tariffs will hinder economic growth and have recently been asking about alternative investments in gold. “Often during times of chaos there is a ‘flight to safety,’ so in a time like this we are seeing some movement to gold as a part of the fear trade.”
According to Baker, who is the founder, owner and president of Apex Financial Services and a member of CNBC’s FA Council, “incorporating gold, and other commodities, is a good idea in general.”
He recommends adding gold ETFs to client portfolios, although “there have been occasions where we have utilized gold stocks in the form of investing in mining companies or gold-related company mutual funds.”
As for physical gold, “if it makes you feel good to go grab an ounce at Costco or wherever, do it,” he said. But with that comes the additional responsibility and costs of storing, insuring and safekeeping those holdings, he added.

IRS offers penalty relief for micro-captive transactions

Transforming accounting firms through connected leadership

You have options if you can’t pay your taxes by April 15

New 2023 K-1 instructions stir the CAMT pot for partnerships and corporations

The Essential Practice of Bank and Credit Card Statement Reconciliation

Are American progressives making themselves sad?
Trending
-

 Accounting1 week ago
Accounting1 week agoOn the move: KPMG adds three asset management, PE leaders
-

 Accounting1 week ago
Accounting1 week agoX asks Supreme Court to shield Coinbase users from IRS probe
-

 Economics1 week ago
Economics1 week agoPresident Donald Trump says Fed Chair Powell should cut interest rates and ‘stop playing politics’
-

 Economics6 days ago
Economics6 days agoTexas looks set to pass America’s biggest school-voucher scheme
-

 Personal Finance1 week ago
Personal Finance1 week agoAmid trade turmoil, ‘you do not want to time the market’
-

 Economics1 week ago
Economics1 week agoChina to impose 34% retaliatory tariff on all goods imported from the U.S.
-

 Personal Finance1 week ago
Personal Finance1 week agoMost credit card users carry debt, pay over 20% interest: Fed report
-

 Finance1 week ago
Finance1 week agoBuffett denies social media rumors after Trump shares wild claim that investor backs president crashing market
